PRE-OPERATIVE RADIOGRAPHIC ASSESSMENT
As with most orthopaedic problems, the initial radiographic evaluation of glenohumeral arthritis is typically done with plain film radiographs. Standard 3-4 view X-rays of the shoulder are obtained including an AP, Axillary, and Scapular-Y view. CT scans are also routinely obtained. While CT scan is often more accurate for performing various pre-operative measurements, one can still gain useful information from the plain films, and many of the radiographic measurements can be performed in a similar fashion to how they would be on the CT scans. The following text and videos will demonstrate how to perform the various radiographic measurements useful in pre-operative assessments in patients with glenohumeral arthritis.
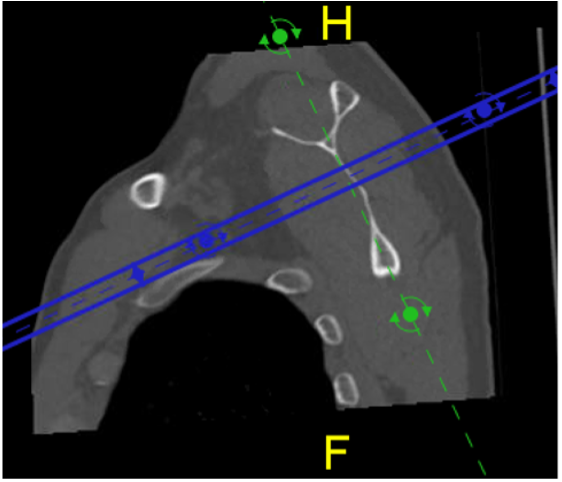
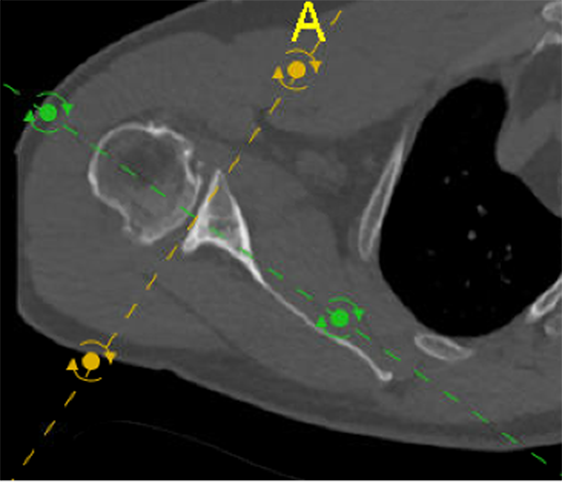
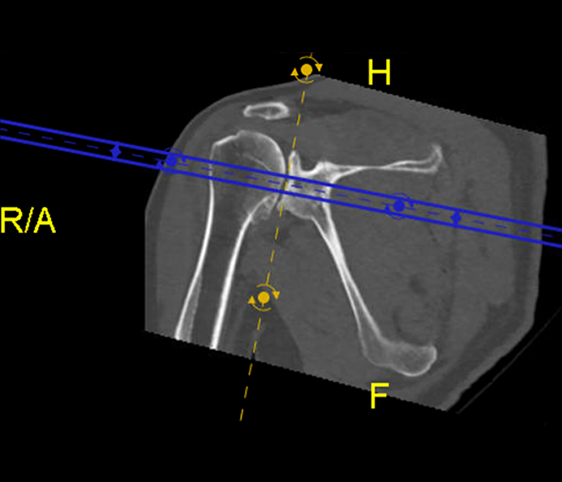
CT Formatting:
To obtain the most accurate measurements from the CT scans, they must be properly formatted to be aligned with the scapula in the sagittal, coronal, and axial planes. This can be accomplished with use of MIP software to reformat the scans appropriately. In the sagittal plane the axis of the scan should be oriented in line with the scapular body. In the axial plane the axis of the scan should be oriented in line with the scapular spine cranially and continuous with the scapular body as one moves caudally. Lastly in the coronal plane the axis should be in line with the face of the glenoid. An example of a CT which has been reformatted to the proper planes is shown below with the green-dotted line representing the properly formatted axis in the sagittal and axial planes and the yellow-dotted line demonstrating the properly formatted axis in the coronal plane.
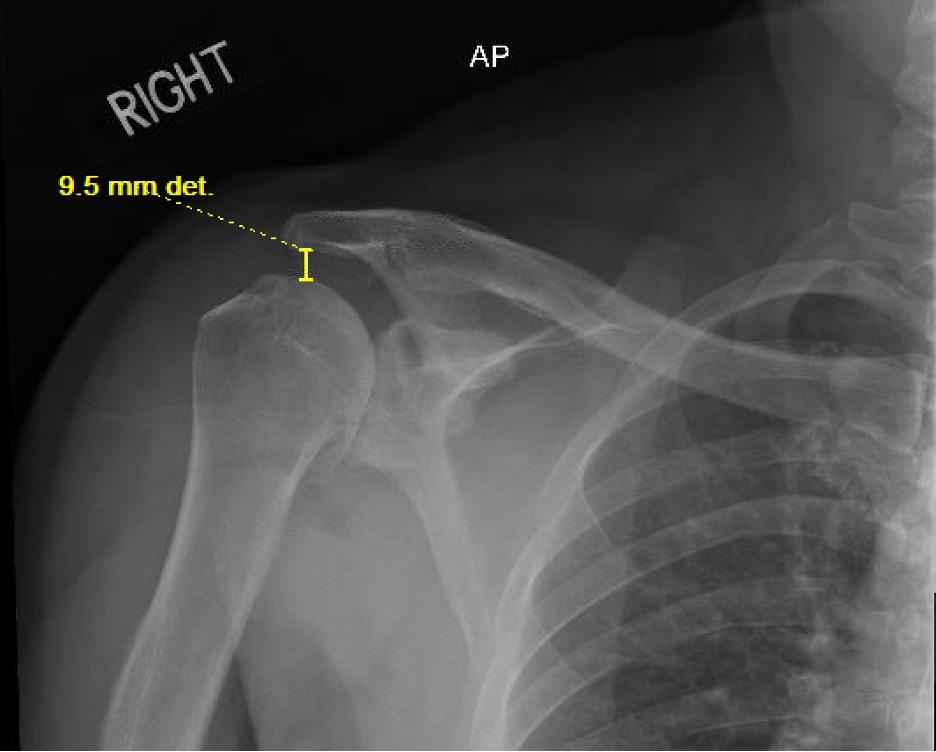
Acromiohumeral Interval
The acromiohumeral interval is defined as the distance from the undersurface of the acromion to the top of the humeral head. It is traditionally described as being performed on a true AP radiograph of the shoulder but has also been described as measured on CT or MRI of the shoulder as well. This interval tells us about the relationship of the humeral head to the glenoid in the superior/inferior plane. A normal range for this distance is 8-12mm. A value of 7mm or less indicates superior humeral head migration and is suggestive of a rotator cuff tear, specifically of the supraspinatus tendon. This is important when considering arthroplasty options because a patient who has a suspected deficiency of the rotator cuff would be a better candidate to receive a reverse total shoulder arthroplasty for reasons previously described. A value of >12mm is indicative of inferior humeral head subluxation or dislocation.
Glenoid Version Angle
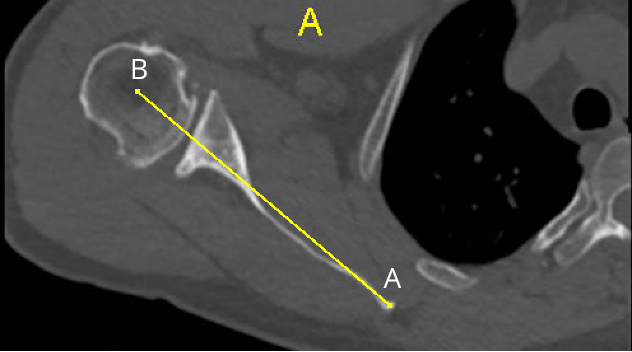
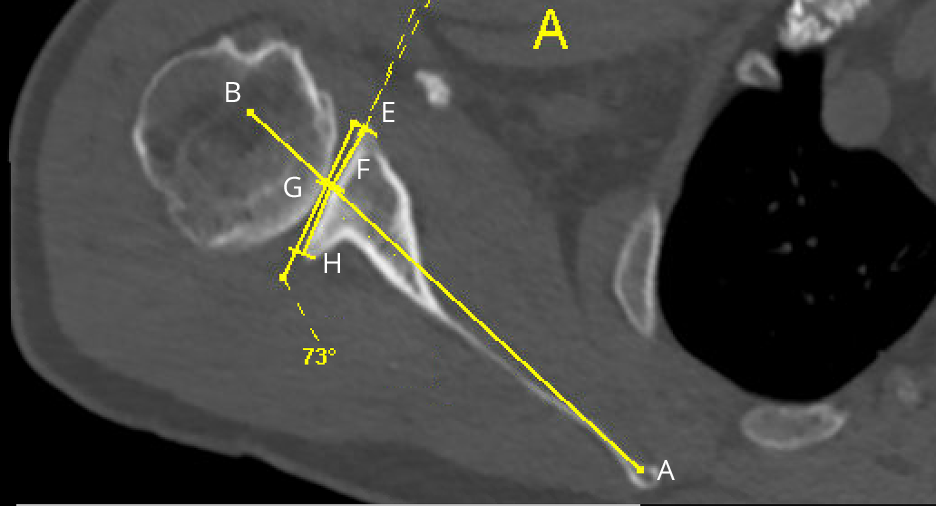
The glenoid version angle measures the amount of anteversion or retroversion present in the glenoid. It is measured characteristically on an axial CT cut through the center of the glenoid but may also be measured on an axial cut MRI. The two main methods to measure this are the Friedman’s line method and the Scapular Body method. Friedman’s line method has shown to have better inter-reader reliability and is the method that will be used in the case examples and practice problems.
Friedman’s line is described as a line drawn down the long axis of the scapula from the tip of the medial border of the scapula (A) through the center of the glenoid vault (B).
To measure the glenoid version angle Friedman’s line is drawn first, and then a second line is drawn across the anterior (C) and posterior (D) margins of the glenoid along the glenoid face. A neutral glenoid version angle is 90 degrees. When the glenoid version angle is not equal to 90 degrees (not neutral), 90 can be subtracted from the measured angle to determine at what angle the glenoid is anteverted or retroverted. A positive glenoid version angle corresponds to glenoid anteversion, and a negative glenoid version angle corresponds to glenoid retroversion. The normal version of the glenoid is +2 to – 10 degrees..
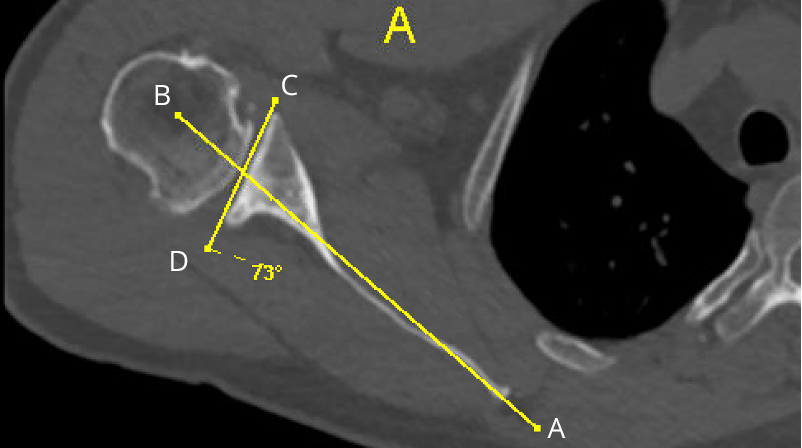
In this example, the glenoid version angle is -17, indicating that the glenoid is 17 degrees retroverted. This obtained by subtracting 73-90 = -17.
X-Ray
CT
In patients with a Bi-concave glenoid, the glenoid angle of the Paleo-glenoid (line E-F) and the Neo-glenoid (line G-H) can be measured individually. These angles are again subtracted from 90 to determine the degree of anteversion/retroversion of the neo/paleo glenoid.
Glenoid version and degree of glenoid bone loss are important aspects of operative planning. In patients with distorted glenoid retroversion, subluxation of the humeral head, and glenoid bone loss this needs to be addressed intra-operatively. High-side reaming, augmented glenoid baseplates, and bone grafting to fill the glenoid defect are strategies to correct glenoid version and address this issue. More can be found on this subject in the Management of Glenoid Bone Loss Section.
Anterior/Posterior Humeral Head Subluxation
Measurement of Anterior or Posterior Humeral Head Subluxation is performed based on the percentage of the humeral head either anterior or posterior to Friedman’s line on an axial CT image in the center of the glenoid. Friedman’s line is drawn first and extended to pass through the humeral head (AB). A second line known as the glenoid fossa line is draw perpendicular to Friedman’s line through the center of the humeral head connecting the anterior and posterior surfaces (CE). The proportion of the humeral head that is either anterior or posterior to the glenoid (CD or DE) is divided by the total Anterior-Posterior distance of the humeral head (CE) and multiplied by 100 to determine percentage of subluxation ((CD or DE/(CD +DE)) x 100).
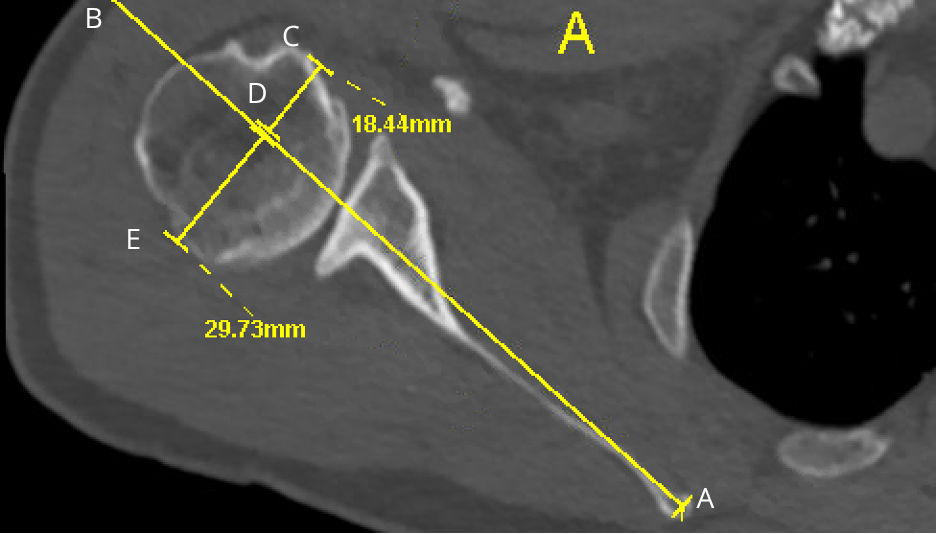
In this example the total A to P (CD + DE) distance of the humeral head is 48.17mm (18.44 + 29.73). The portion of the humeral head that is posterior to Friedman’s line is 29.73 (DE). Therefore, the amount of humeral head is ((29.73/48.17) x100) = 62%. In this case the subluxation is posterior.
X-Ray
CT
Glenoid Inclination Angle
Measurement of glenoid inclination is performed on a coronal plane CT. A line (AB) is drawn down the axis of the supraspinatus fossa and a second line known as the glenoid fossa line is drawn along the glenoid face from the superior to inferior margin (CD). A neutral glenoid inclination is 90 degrees. When the glenoid inclination is not equal to 90 degrees (not neutral), 90 may be subtracted from the measured angle to determine at what angle the glenoid is superiorly or inferiorly inclined. A positive glenoid inclination corresponds to superior glenoid inclination, and a negative glenoid inclination corresponds to an inferior glenoid inclination. The normal glenoid inclination is 1-10 degrees of superior inclination.
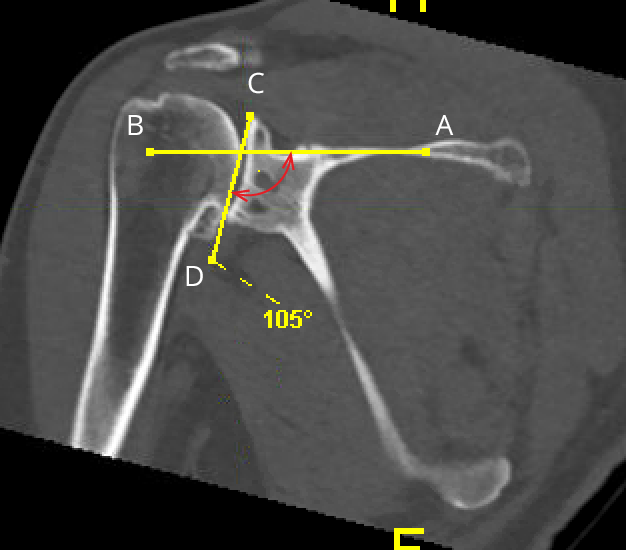
The angle measured is 105 degrees. Therefore to obtain glenoid inclination angle: 105-90=15. In this example the glenoid version angle is 15 degrees of superior inclination.
X-Ray
CT
Superior/Inferior Humeral Head Subluxation
Measurement of Superior or Inferior Humeral Head Subluxation is performed based on the percentage of the humeral head either superior or inferior to a line (AB) drawn down the middle of the glenoid on coronal CT image in the center of the glenoid. A second line is draw perpendicular to the line down the supraspinatus fossa through the center of the humeral head connecting the superior surface to the level of the surgical neck (CE). The proportion of the humeral head that is either superior or inferior to the glenoid (CD or DE) is divided by the total Superior-inferior distance of the humeral head (CE) and multiplied by 100 to determine percentage of subluxation ((CD or DE/(CD + DE)) x 100).
.
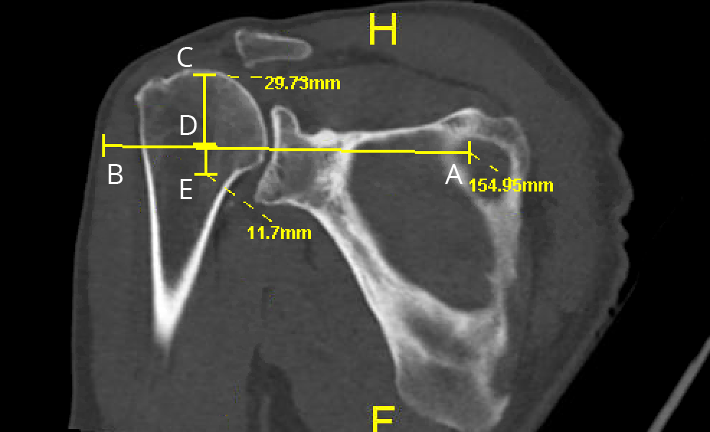
In this example, the total distance (CE) is 41.43. (29.73 (CD) + 11.7 (DE) = 41.43) The distance CD is larger than DE therefore the formula for calculation of humeral head subluxation is (CD/(CD + DC)) x 100. (29.73/41.43) x 100 = 71.75%. This means that the humeral head is superiorly subluxed.
X-Ray
CT
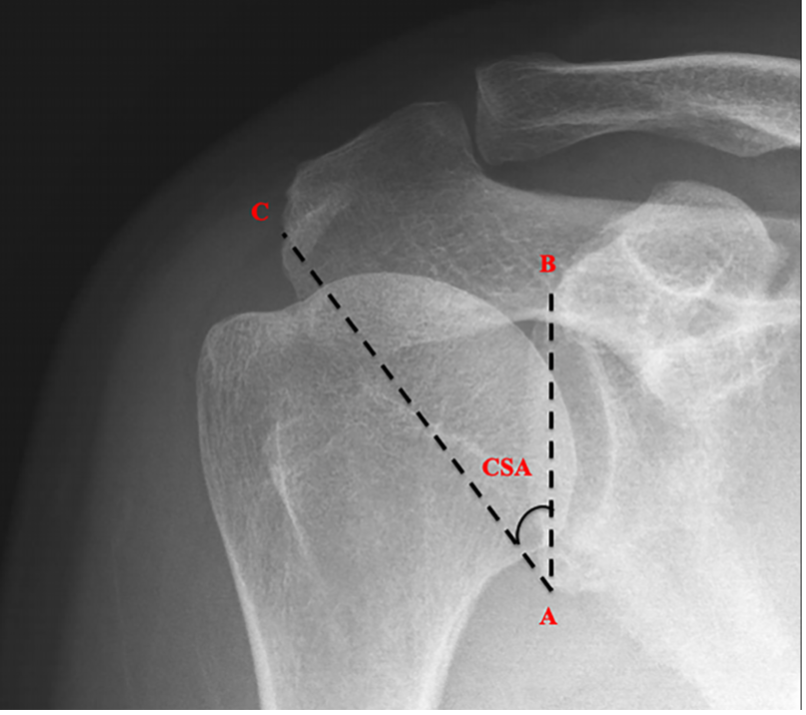
Critical Shoulder Angle (CSA)
Critical shoulder angle is defined as the angle formed between the plane of the face of the glenoid and the line connecting the lateral most border of the acromion as seen on true AP radiograph of the shoulder. Normal is said to range from 30-35 degrees. Smaller CSA’s have been found to be associated with osteoarthritis, and larger CSA’s have been found to be associated with rotator cuff pathology.
.