INTRODUCTION
When evaluating patients with glenohumeral arthritis, multiple factors play a role in determining treatment modality. Patient characteristics such as age, sex, activity level, and medical comorbidities all play a role in decision making. In the ensuing text, we will mainly focus on anatomic and radiographic considerations as they are related to treatment.
Total shoulder arthroplasty was thought to be pioneered by Jules Emile Pean in 1893 when he replaced the shoulder in a 37-year-old patient with tuberculous arthritis with platinum and rubber components. The conception of the modern total shoulder replacement was attributed to Neer in the 1950’s when he began performing proximal humeral replacement also known as hemiarthroplasty for traumatic and degenerative changes of the glenohumeral joint. Neer’s work expanded to include the addition of a glenoid component which was shown to improve pain relief in patients with degenerative changes on the glenoid side of the glenohumeral joint and was the foundation for which the modern anatomic total shoulder prostheses are based.
Despite generally good outcomes of anatomic total shoulder arthroplasty, it was noticed that outcomes were poorer in patients who had deficiency of the rotator cuff musculature. Reverse total shoulder arthroplasty was originally designed as a solution to the shortcomings of the Neer total shoulder prosthesis specifically in patients with rotator cuff deficiency. The Mark I was the first reverse total shoulder prosthesis and was a highly constrained design in which the glenoid and humeral components were “reversed” so that the glenoid component was the spherical component, and the humeral component was the cup. This design was modified and expanded upon to resemble the reverse total shoulder prosthesis we have today.
A fixed, distalized, and medialized center of rotation of the glenohumeral joint along with the inherent stability of the prosthesis and altered lever arm of the deltoid muscle allow the deltoid to function throughout the entire arc of motion during shoulder abduction with a reverse total shoulder arthroplasty, thus allowing the deltoid to compensate for the deficient rotator cuff. We will discuss biomechanics of reverse total shoulder arthroplasty further in the Biomechanics of Reverse Total Shoulder Arthroplasty section.
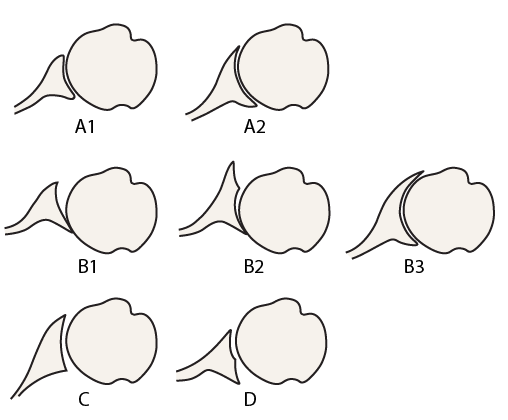
Another consideration aside from rotator cuff integrity when determining which arthroplasty option is more appropriate for each patient is glenoid morphology and the presence or absence of glenoid bone loss. The original classification by Walch et al. was proposed in 1999 and has since been modified to include four types of glenoid morphology A-D with various subtypes in each of the groups based on morphologic appearance in the axial plane.
Walch Classification
Type A – Centered humeral head with concentric glenoid wear and no subluxation of the humeral head
- A1 – minor central erosion
- A2 – major central erosion with the humeral head protruding into the glenoid cavity
Type B – posterior subluxation of the humeral head with asymmetric glenoid wear
- B1 – narrowing of the posterior joint space, subchondral sclerosis, osteophytes
- B2 – biconcave glenoid with posterior rim erosion and glenoid retroversion
- B3 – monoconcave glenoid with significant posterior wear, typically with >25 degrees of glenoid retroversion
Type C – Dysplastic glenoid with >25 degrees of glenoid retroversion regardless of glenoid erosion
Type D – Glenoid anteversion with anterior glenoid wear and anterior humeral head subluxation
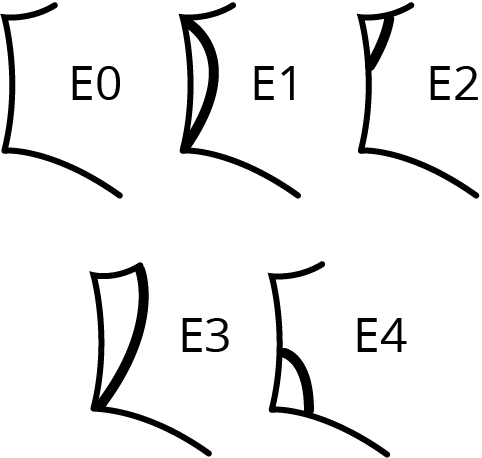
Favard Classification
E0 – No glenoid erosion
E1 – Central glenoid erosion
E2 – Glenoid erosion predominantly in the superior pole
E3 – Global glenoid erosion more severe in the superior pole
E4 – Glenoid erosion predominantly in the inferior pole
The foundation of radiographic evaluation of patients with glenohumeral arthritis is based on the Walch and Sirveaux classifications. Multiple radiographic measurements have been described and provide further detail and objective numbers which are useful when evaluating a patient for surgery as well as in pre-operative planning. We will discuss these next.